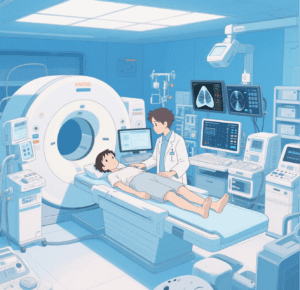
In the interventional operating room of a top-tier tertiary hospital in Beijing, a vascular interventional robot is precisely moving a catheter along a preset path. The repeat positioning accuracy of its mechanical arm reaches 0.05 millimeters, and the doctor perceives vascular resistance through the force feedback system of the console. The radiation exposure during the entire operation is 70% lower than that of traditional methods. In the adjacent laboratory, a fully automated biochemical testing line processes 1,800 samples per hour, with results transmitted in real time to the doctor’s workstation via the LIS system — the evolution of medical automation equipment is safeguarding life and health with technical precision while balancing medical efficiency with humanistic care.
Breakthroughs in automation in the surgical field have always centered on “ultra-precise operations” and “minimally invasive treatment.” Traditional open surgery relies on the stability of the doctor’s hands, but orthopedic surgical robots, guided by intraoperative CT, can control the error of screw implantation within 0.3 millimeters. Data from a spinal surgery team shows that after adopting robot-assisted surgery, the incidence of postoperative complications in patients dropped from 8% to 2.3%. Even more remarkable is the realization of remote surgery: through high-definition images and mechanical arm motion signals transmitted via 5G networks, experts can control surgical robots thousands of miles away to perform routine surgeries such as cholecystectomy, with signal delay controlled within 20 milliseconds — almost indistinguishable from on-site operations. This brings high-quality medical resources to patients in remote areas.
In laboratory testing, automation equipment is resolving the contradiction between “efficiency and precision.” In traditional manual testing, the error rate of sample pipetting is about 3%, while fully automated sample processing systems, which control the piston movement of pipettes via servo motors, can limit errors to within 0.5%. After a third-party testing institution introduced a fully automated nucleic acid extraction instrument, the number of samples processed per batch increased from 96 to 384, testing time was shortened by 60%, and sample contamination caused by manual operations was avoided. For special samples, automation equipment can also achieve customized processing: automated blood culture systems can alert as soon as bacteria grow, reducing the diagnosis time for sepsis from 48 hours to 6 hours, winning a critical window for emergency treatment.
Automation in pharmaceutical production is a core barrier to ensuring drug safety. In biopharmaceutical workshops, fully automated filling lines use negative pressure isolation technology to control the particle concentration in sterile areas to less than 10 particles per cubic meter. The filling accuracy of vials reaches ±0.01 milliliters, and each drug is equipped with a unique electronic traceability code, enabling full tracking of production and circulation links. Data from a vaccine manufacturer shows that after introducing an automated freeze-dried preparation production line, the sterility pass rate of products increased from 99.5% to 99.99%, and production efficiency tripled. More importantly, automated systems can precisely control parameters such as the temperature and pH value of fermentation tanks, limiting fluctuations in the content of active ingredients in biopharmaceuticals to within 5% to ensure stable efficacy.
The uniqueness of medical automation lies in maintaining a balance between “technology-assisted humanity.” Although surgical robots can operate with precision, the final treatment plan is still formulated by doctors based on the patient’s condition; while laboratory automation equipment can produce results quickly, the interpretation of abnormal data still relies on the professional judgment of laboratory technicians. Practice in an oncology hospital shows that in radiotherapy planning, AI automated systems can generate preliminary plans within 10 minutes, but doctors adjust them based on factors such as the patient’s age and physical fitness, improving treatment outcomes by 15% while reducing the incidence of adverse reactions.
In the future, with the development of flexible robots, non-invasive sensing, and other technologies, medical automation equipment will move toward “higher precision, more minimally invasive, and smarter” capabilities: swallowable micro-robots can deliver drugs precisely in the digestive tract; exoskeleton robots controlled by brain-computer interfaces can help paraplegic patients stand again; even automated diagnostic systems in different hospitals can share case data to form cross-regional diagnosis and treatment networks. However, no matter how technology evolves, the ultimate goal of medical automation remains “making healthcare more accessible, safer, and more humane” — the precision of equipment and the kindness of doctors complement each other, jointly safeguarding the dignity of life.
#craftsman automation share price #robotic process automation #jyoti cnc automation share price