Artificial intelligence (AI) and automation are driving a paradigm shift in pharmacy practice, unlocking new potentials to elevate clinical care quality, optimize operational efficiency, and redefine the value of pharmacy teams. While nearly 50% of global healthcare organizations aim to integrate AI into pharmacy workflows by 2025, successful adoption is not merely a technical task—it requires clear alignment of stakeholder roles, actionable insights into tangible benefits, and proactive mitigation of implementation barriers. This article is tailored for clinicians, pharmacy students, and healthcare administrators, offering a structured overview of technological advancements, workforce implications, and educational imperatives in the rapidly evolving landscape of intelligent pharmacy.
AI and Automation: Reshaping Hospital and Retail Pharmacy Operations
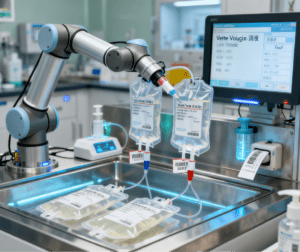
Today’s pharmacies—whether in hospitals or retail settings—are leveraging AI and automation to replace manual, repetitive tasks with precise, scalable solutions, while freeing up pharmacists to focus on high-value clinical work.
In hospital pharmacy settings, technology has become integral to core workflows:
Automated dispensing cabinets (ADCs) enable secure, real-time medication access at the point of care, reducing medication retrieval time by up to 30%.
Robotic intravenous (IV) compounding systems minimize human error in sterile drug preparation, cutting waste by 25% and enhancing supply chain resilience.
Radio frequency identification (RFID) inventory systems automate stock tracking, lowering inventory holding costs by 18% and eliminating stockouts of critical medications.
AI-driven analytics further optimize care: 87.3% of hospitals now use data from smart pumps, clinical decision support (CDS) tools, or dispensing automation to flag potential errors. Additionally, 73% of hospitals have adopted innovative prescription verification tools—these systems enable remote oversight of low-risk prescriptions (e.g., routine antibiotics) with auto-approval, while routing high-alert medications (e.g., opioids, chemotherapy drugs) to pharmacists for manual review, striking a balance between efficiency and safety.
In retail pharmacy settings, automation is being deployed at scale to handle growing prescription volumes:
CVS Health uses centralized AI and robotic hubs to serve over 9,000 stores, processing 50% of its prescriptions through automated systems and reducing dispensing errors by 60%.
Walgreens’ robotic filling centers now handle 60% of prescriptions for 3,000+ stores, cutting patient wait times by an average of 15 minutes.
Walmart’s automated pharmacy facilities process 100,000 prescriptions daily, with plans to support 90% of its stores by 2026—this scale not only boosts throughput but also reduces manual error rates to near zero.
Tangible Benefits: For Patients, Pharmacists, and Health Systems
The integration of AI and automation delivers multi-layered value across the healthcare ecosystem, with impacts ranging from improved patient outcomes to enhanced workforce retention.
For Patients: Safer, Faster, More Personalized Care
Reduced medication errors: Centralized automated filling systems lower dispensing error rates to <0.1%, compared to 2–3% with manual methods.
Shorter wait times: Retail pharmacies with automation report 20–30% faster prescription turnaround, while hospital ADCs cut medication delivery time to patient units by 40%.
Higher satisfaction: Healthcare systems with automated pharmacies see a 15–22% improvement in pharmacy-related patient satisfaction scores, driven by faster service and more time spent with pharmacists.
For Pharmacists: From “Dispensers” to “Clinical Care Partners”
The most transformative benefit is the reshaping of pharmacist roles:
Increased clinical time: In automated environments, pharmacists spend 45% more time on patient-facing care—such as medication therapy management (MTM) for chronic conditions (e.g., diabetes, hypertension), counseling on medication adherence, and collaborating with physicians on treatment plans.
Boosted productivity: Automation reduces time spent on counting pills, labeling, and inventory checks by up to 33%, allowing pharmacists to manage more complex cases without burnout.
Career advancement: Access to AI tools (e.g., CDS for drug interactions) and automated workflows enables pharmacists to pursue advanced roles, such as ambulatory care pharmacists or medication safety officers.
For Health Systems: Efficiency + Workforce Resilience
Cost savings: Automation reduces labor costs associated with routine tasks by 12–18%, while RFID inventory systems cut waste from expired or overstocked medications by 20%.
Retention strategy: Amid widespread pharmacy workforce shortages, AI and automation reduce workload strain—health systems with automated pharmacies report 25% lower pharmacist turnover rates, as staff are less likely to experience burnout and more likely to engage in meaningful clinical work.
Navigating Challenges: Cost, Resistance, and Cybersecurity
While the benefits are clear, integrating AI and automation into pharmacies is not without hurdles. Addressing these proactively is critical to avoiding failed implementations.
- Upfront Costs and Resource Requirements
Smaller hospitals or independent pharmacies often struggle with the high initial investment: robotic IV compounding systems can cost $500,000–$1 million, and EHR integration for AI tools may require additional IT resources. Solutions for smaller institutions include:
Partnering with regional health systems to share automated hubs (e.g., shared robotic filling centers for independent pharmacies).
Seeking government or private grants for healthcare technology adoption (e.g., the U.S. Health Resources and Services Administration’s Pharmacy Quality Improvement Program).
- Stakeholder Resistance to Change
Pharmacy teams and clinical partners may resist automation due to fears of job displacement or discomfort with new technology. Mitigation strategies include:
Early engagement: Involve pharmacists in technology selection (e.g., testing robotic systems before purchase) to ensure tools align with workflow needs.
Role clarity: Emphasize that automation “enhances, not replaces” pharmacists—framing technology as a tool to eliminate tedious tasks and enable clinical focus.
Targeted training: Offer hands-on workshops (e.g., “AI for Medication Safety”) to build confidence in using new tools.
- Cybersecurity and Ethical Risks
As pharmacies rely more on cloud-based AI and connected devices (e.g., smart pumps, RFID systems), protecting sensitive patient data becomes paramount:
Health systems must implement end-to-end encryption for prescription data and regular cybersecurity audits for AI tools.
Algorithmic transparency is critical: Pharmacies should validate AI outputs (e.g., CDS alerts) against clinical guidelines and monitor for biases (e.g., underrepresentation of marginalized populations in training data) to avoid flawed recommendations.
Preparing the Next Generation of Pharmacists for the AI Era
Pharmacy students and early-career professionals must be equipped to thrive in technology-driven environments. Pharmacy education programs need to evolve in three key ways:
- Integrate Digital Literacy into Curricula
Courses should move beyond traditional clinical training to include:
Hands-on training in data interpretation (e.g., using pharmacy dispensing data to identify adherence gaps).
Practical skills in AI tool use (e.g., interpreting AI-generated drug interaction alerts, optimizing automated dispensing workflows).
Health informatics basics (e.g., integrating automated systems with EHRs to streamline care coordination).
- Foster Interdisciplinary Collaboration
Pharmacists increasingly work with data scientists, IT teams, and clinicians to implement AI tools. Educational programs should:
Offer interdisciplinary electives (e.g., “AI in Healthcare Teams”) that pair pharmacy students with computer science or nursing students.
Teach advocacy skills for evidence-based AI deployment (e.g., how to justify AI investments to hospital administrators).
- Expand Experiential Rotations
Clinical rotations should include placements in AI-enhanced settings, such as:
Walmart’s automated prescription hubs.
Hospital-based robotic IV compounding units.
Pharmacies using AI for MTM (e.g., AI-driven patient adherence monitoring).
These experiences help students bridge the gap between theory and practice, preparing them to lead AI integration in future roles.
Future Directions: Strategic Integration and Ethical Leadership
As AI technology advances, its role in pharmacy will expand beyond operational efficiency to clinical innovation:
Advanced clinical support: AI tools will assist with complex tasks like real-time literature analysis (e.g., OpenEvidence, which provides evidence-based recommendations for off-label drug use) and personalized patient education (e.g., AI-generated multilingual medication guides).
Predictive analytics: AI will enable proactive care—for example, predicting medication non-adherence using patient data (e.g., refill history, social determinants of health) and alerting pharmacists to intervene.
Yet, AI remains a tool—not a replacement for pharmacists. The human element—empathy, clinical judgment, and patient advocacy—remains irreplaceable. Pharmacists must serve as “guardians of clinical relevance,” ensuring that AI tools are validated against real-world patient outcomes and that ethical considerations (e.g., patient privacy, equity) guide implementation.
Conclusion
AI and automation are not just transforming pharmacy workflows—they are redefining the profession’s role in healthcare. By reducing errors, freeing pharmacists for clinical work, and improving patient satisfaction, these technologies offer a path to a more efficient, patient-centered pharmacy practice. However, success requires more than technology: it demands a balanced approach that addresses costs, mitigates resistance, and invests in workforce development.
For the pharmacy profession to lead this transformation, stakeholders must collaborate: healthcare administrators need to prioritize evidence-based AI investments, educators must prepare students for digital practice, and pharmacists must embrace technology as a tool to deliver higher-quality care. In doing so, intelligent pharmacy will not only enhance operational efficiency—it will ensure that pharmacists remain vital partners in improving patient health for years to come.