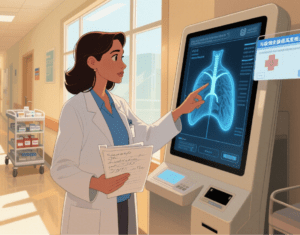
In the quiet of a hospital hallway, Dr. Elena Ruiz pauses over a patient’s chart, her pen hovering. The scan shows a suspicious shadow in the lung—a finding that could mean early cancer, but might also be a harmless artifact of the imaging. Beside her, a screen glows: an AI tool has flagged the anomaly, cross-referencing it with thousands of similar cases and noting, “High correlation with adenocarcinoma in patients with this smoking history.”
- Dr. Ruiz nods, then pulls up the patient’s full history—something the AI can’t do alone. “It’s not telling me what to do,” she says later. “It’s giving me more to work with.”
This is the promise of augmented intelligence in medicine: not a replacement for the human judgment that defines clinical care, but a partner that amplifies it. Unlike artificial intelligence, which often conjures images of machines acting independently, augmented intelligence (AI) centers on collaboration—designing tools that enhance clinicians’ skills, lighten their load, and ultimately improve patient outcomes. It’s a distinction the American Medical Association (AMA) has championed, framing it as a guiding principle for how technology should integrate into health care.
Artificial Intelligence vs. Augmented Intelligence: A Critical Distinction
The AMA House of Delegates didn’t coin “augmented intelligence” by accident. The term is a deliberate reframing of “artificial intelligence,” shifting the focus from technology that might supplant humans to tools that support them.
If artificial intelligence can feel like a black box—making decisions with little explanation—augmented intelligence is a transparent collaborator. It surfaces patterns in data, suggests next steps, or automates tedious tasks, but leaves the final call to the physician.
“Augmented intelligence is about extending human capability, not replacing it,” says Dr. Rahul Khurana, a member of the AMA’s AI Advisory Group. “A radiologist might miss a tiny fracture in a flood of scans; AI can flag it. But only the radiologist can weigh that finding against the patient’s pain, medical history, and life circumstances to decide what happens next.”
This balance—technology as a helper, not a decider—lies at the heart of how the AMA approaches health care AI.
- AMA Policy: Guiding AI Toward Ethical, Equitable Care
As AI tools multiply in clinics and hospitals—from diagnostic algorithms to administrative assistants—the AMA has moved to ensure they serve patients and clinicians alike. Its latest policy, released in 2024, outlines guardrails for development, deployment, and use, with a focus on keeping health care human-centered.
- Key pillars include:
Oversight: Ensuring AI tools are rigorously tested for safety and effectiveness before entering clinical settings, with ongoing monitoring to catch biases or errors.
Transparency: Requiring clear disclosure to both physicians and patients about when AI is used, how it works, and its limitations. A patient deserves to know if an AI flagged their test result—and a doctor needs to understand the tool’s logic to trust it.
Generative AI governance: Addressing the unique risks of tools like ChatGPT, which can generate clinical notes or treatment suggestions but may produce inaccurate information. The policy calls for strict validation of such tools in clinical contexts.
Liability and privacy: Clarifying that physicians aren’t solely responsible for AI errors, as long as they use tools appropriately, and safeguarding patient data from breaches in AI systems.
Equity: Ensuring AI tools work for all populations—regardless of race, gender, or socioeconomic status—by avoiding biased training data that might misdiagnose marginalized groups.
“The goal isn’t to slow down innovation,” explains Dr. Lisa Patel, who helped draft the policy. “It’s to make sure innovation serves everyone. AI can’t just work in wealthy urban hospitals; it needs to help a rural doctor with a small clinic, or a pediatrician navigating a complex case.”
- Physicians on AI: Optimism Grows, but Concerns Linger
Physicians are voting with their keyboards: In 2024, 66% reported using AI tools in their practice—nearly double the 38% who did so in 2023. And enthusiasm is rising too, with 68% seeing clear advantages, up from 65% the year prior.
Much of this excitement stems from AI’s ability to tackle the “paperwork burden” that weighs on clinicians. AI tools now draft progress notes, code diagnoses, or coordinate referrals, freeing doctors to spend more time with patients.
Dr. James Lee, a family physician in Ohio, uses an AI assistant to transcribe patient visits. “I used to spend an hour after hours typing notes,” he says. “Now I hit ‘summarize,’ tweak a few lines, and go home. It’s not glamorous, but it’s life-changing.”
Yet skepticism endures. Many physicians worry about relying on tools with unproven clinical evidence. “I’ll use AI to flag drug interactions, but I still check the pharmacy database myself,” says Dr. Maria Gonzalez, an internist in Texas. “I need to know the tool’s been tested on patients like mine—older adults with multiple chronic conditions—not just healthy 30-year-olds in a lab.”
Other top concerns include data privacy (will AI systems protect sensitive patient info?) and liability (who’s at fault if an AI makes a mistake?). These gaps help explain why, despite growing
use, many physicians say they need more guidance—training on how to integrate AI into workflows, and research proving tools deliver better outcomes.
- The Future: Augmented Intelligence as a Force for Good
In the end, augmented intelligence in medicine is a story about partnership. It’s the radiologist who uses AI to sift through scans but relies on their own eyes to confirm a diagnosis. The pediatrician who lets AI suggest treatment plans but adjusts them based on a parent’s concerns. The clinic staff who uses AI to streamline billing but still picks up the phone to help a confused patient.
The AMA’s policies, and physicians’ growing embrace of these tools, point to a future where technology doesn’t erode the human connection in health care—it strengthens it.
As Dr. Khurana puts it: “Augmented intelligence isn’t about making medicine easier. It’s about making it better—more accurate, more equitable, more focused on the people at its center.”For
patients and clinicians alike, that’s a future worth building.
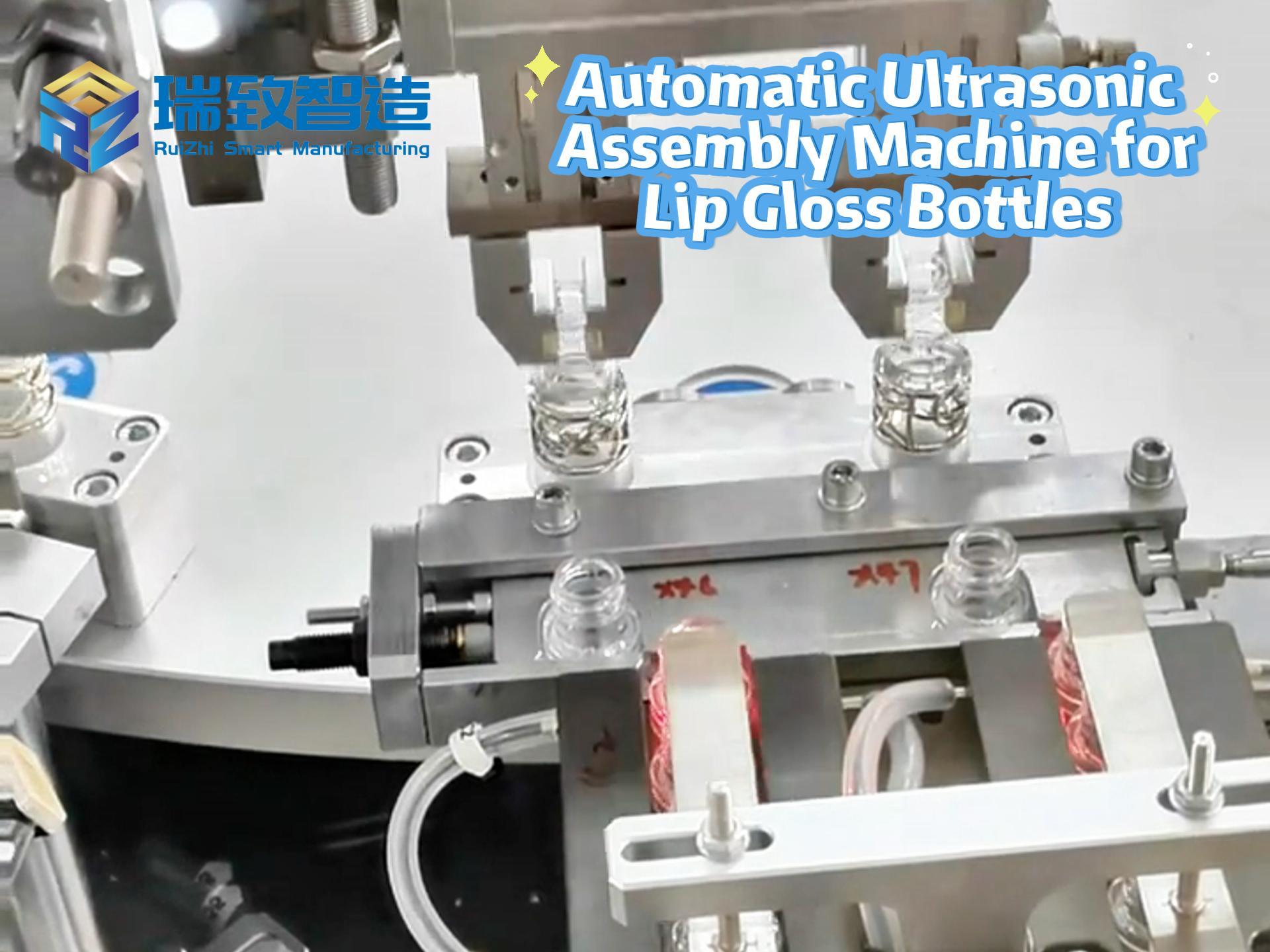
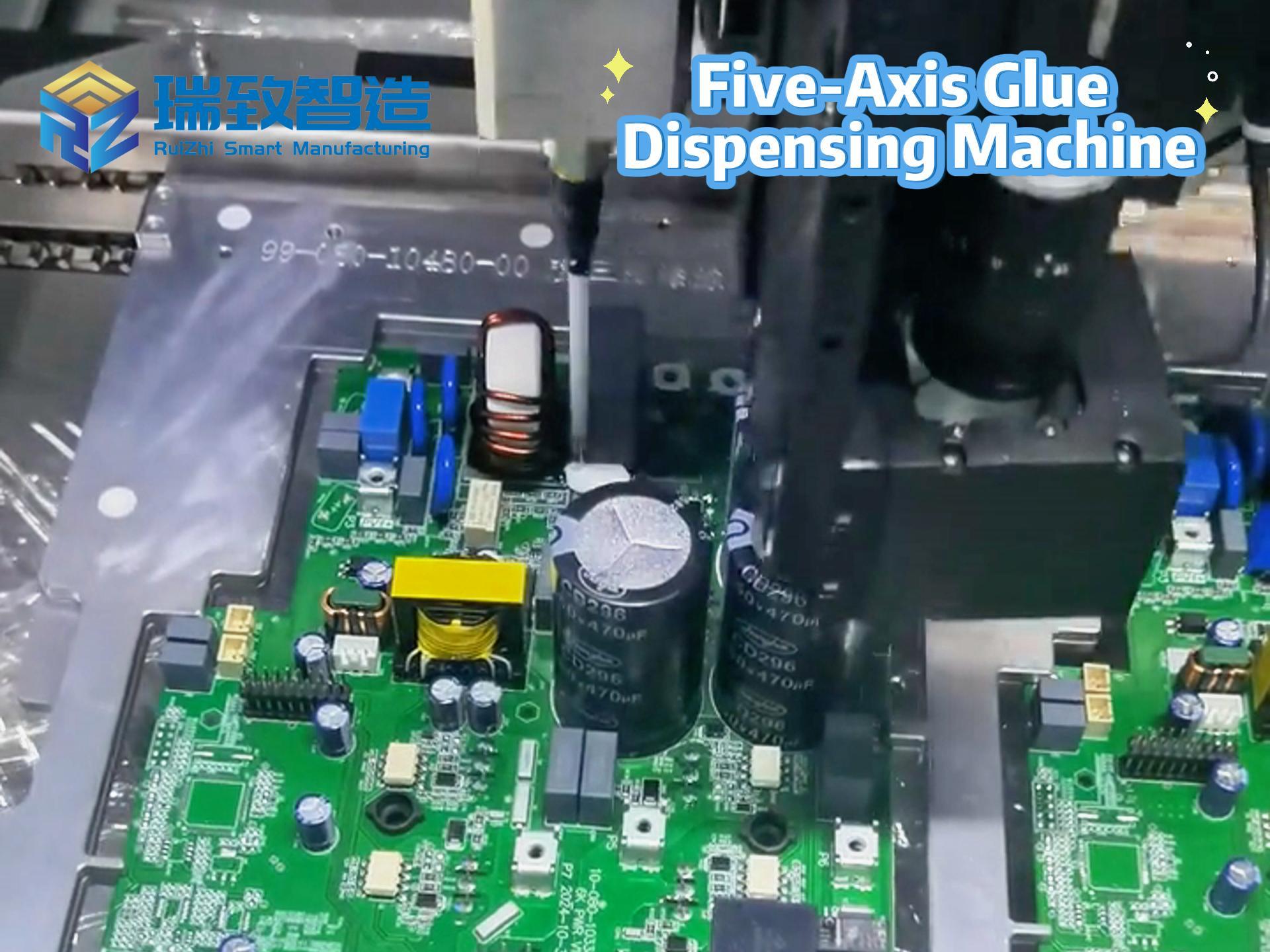
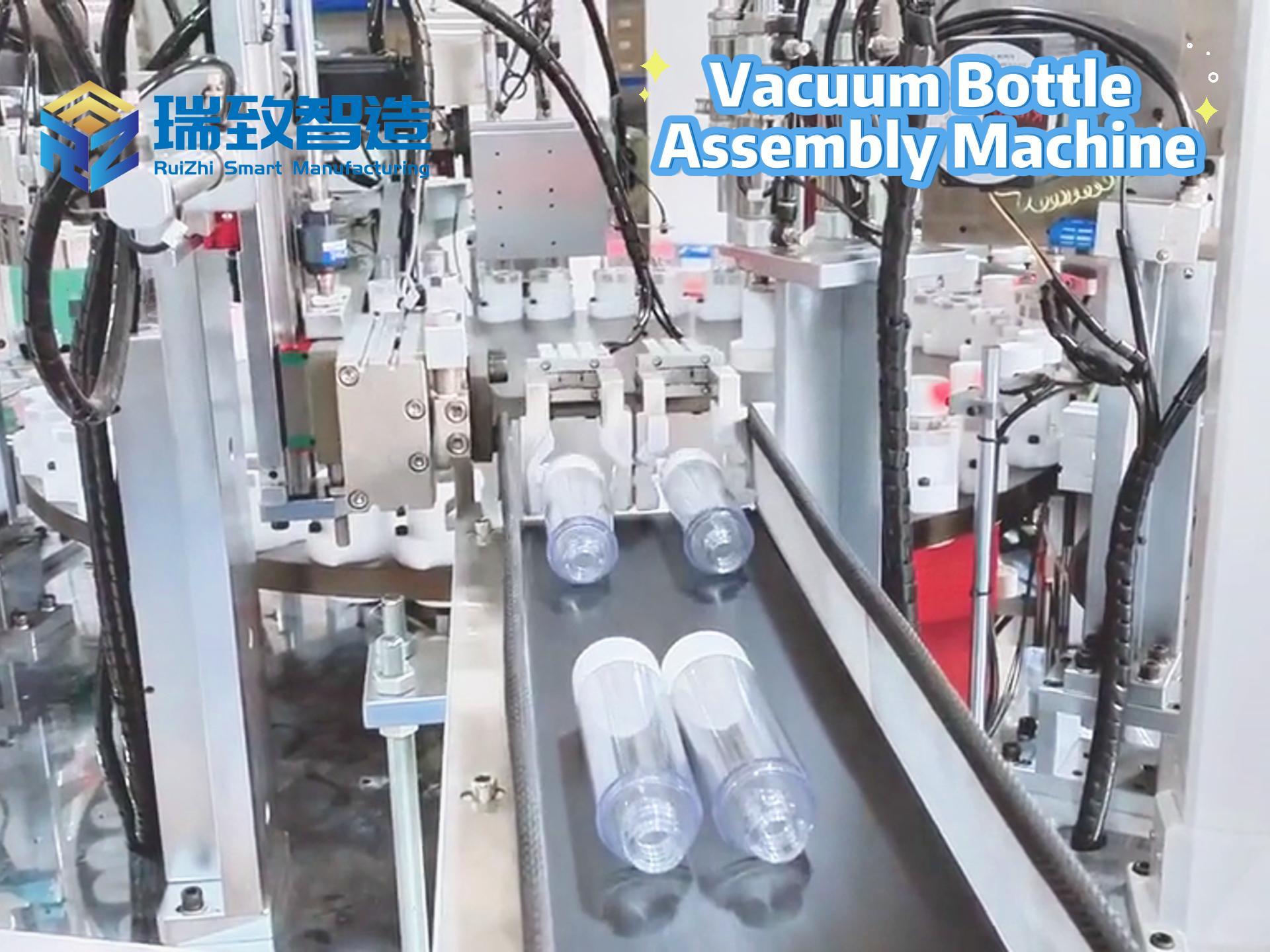
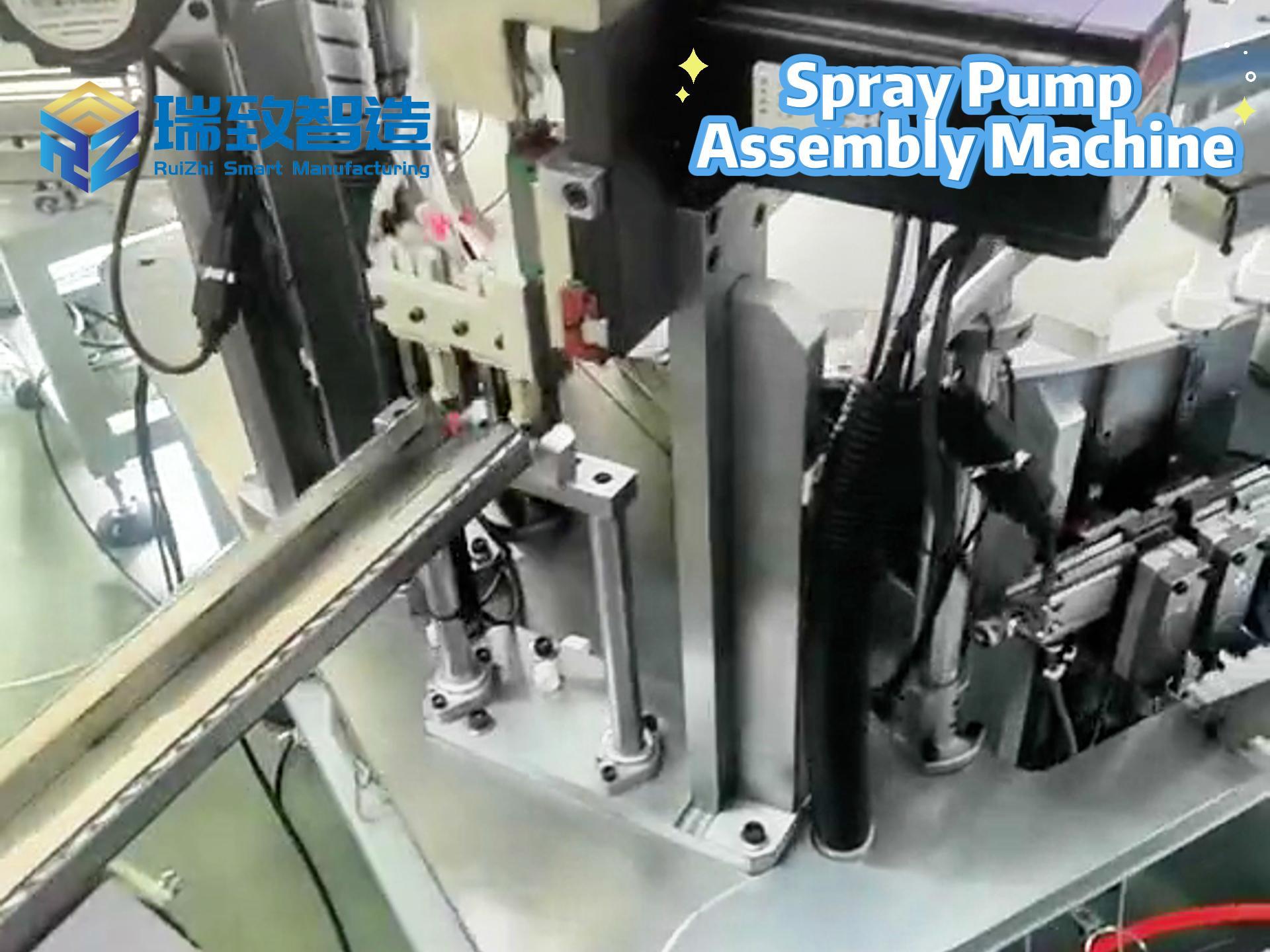
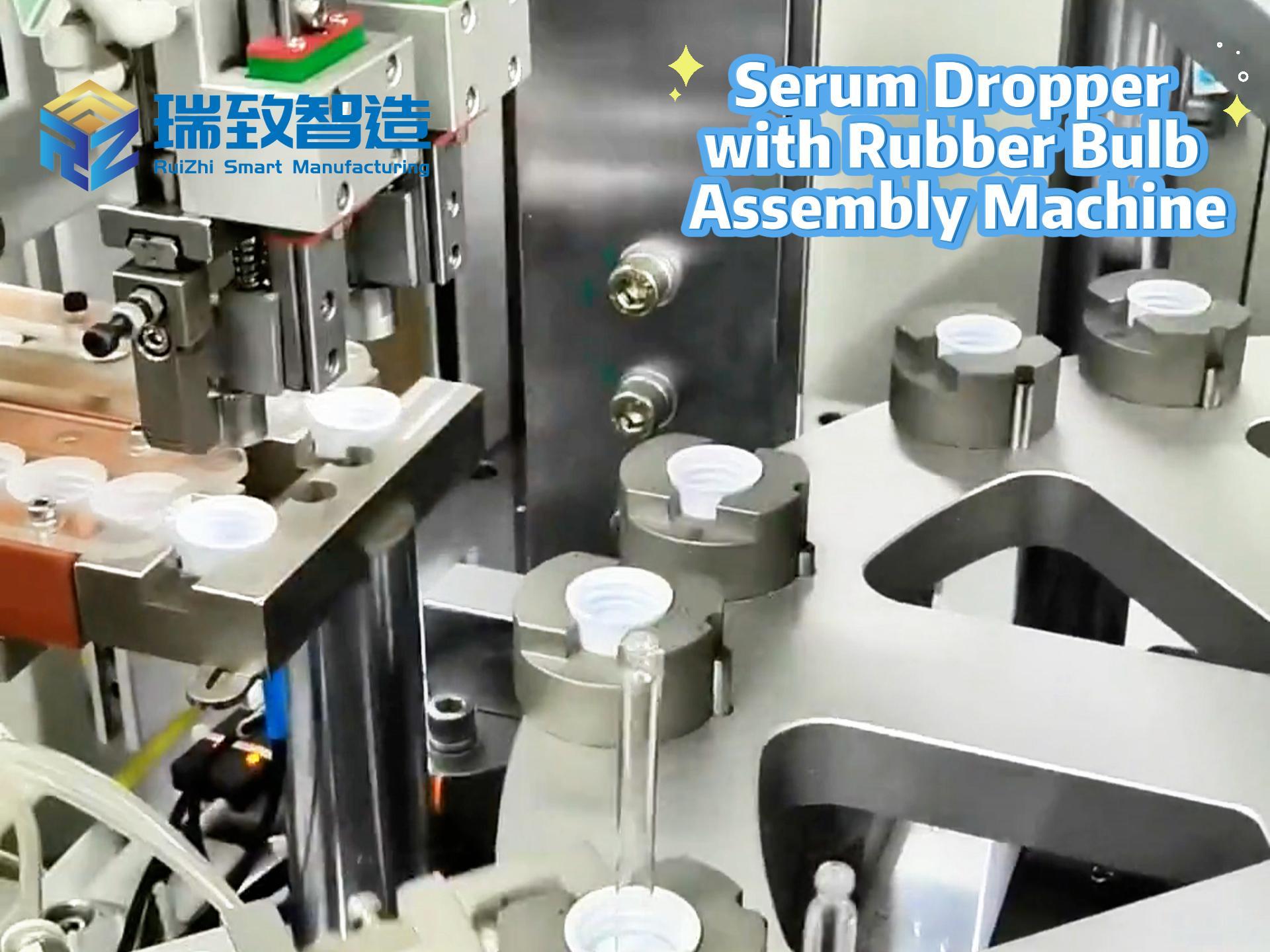
What are the advantages of the automatic motor assembly production line?
The working principle of the automatic motor assembly production line